Natural Immunity vs. Vaccine-Induced Immunity
Israeli pre-print presents evidence that if you got COVID and survived, you have stronger immunity against Delta than those who were simply vaccinated.
Yesterday, we saw a pre-print drop on medRxiv titled "Comparing SARS-CoV-2 natural immunity to vaccine-induced immunity: reinfections versus breakthrough infections" from a research team based out of Israel.
We'll go through the paper in greater detail but the tl;dr is the results suggest that natural infection affords longer-lasting and stronger protection against infection, symptomatic disease, and hospitalization due to the SARS-CoV-2 Delta variant.
Here's a quick summary:
- Researchers were studying how natural immunity compared to vaccine-induced immunity for SARS-CoV-2.
- The longitudinal study had 3 groups: 1) SARS-CoV-2 naïve individuals who received a 2-dose regimen of the Pfizer vaccine 2) Previously infected individuals who were not vaccinated and 3) Previously infected individuals who were vaccinated with a single dose.
- 3 models were evaluated: 1) previously infected vs. vaccinated individuals 2) SARS-CoV-2 naïve vaccinees to unvaccinated, previously infected individuals and 3) previously infected individuals vs. previously-infected-and-once-vaccinated individuals.
The results were as follows (emphasis mine):
SARS-CoV-2-naive vaccinees had a 13.06-fold (95% CI, 8.08 to 21.11) increased risk for breakthrough infection with the Delta variant compared to those previously infected, when the first event (infection or vaccination) occurred during January and February of 2021. The increased risk was significant (P<0.001) for symptomatic disease as well. When allowing the infection to occur at any time before vaccination (from March 2020 to February 2021), evidence of waning natural immunity was demonstrated, though SARS-CoV-2 naive vaccinees had a 5.96-fold (95% CI, 4.85 to 7.33) increased risk for breakthrough infection and a 7.13-fold (95% CI, 5.51 to 9.21) increased risk for symptomatic disease. SARS-CoV-2-naive vaccinees were also at a greater risk for COVID-19-related-hospitalizations compared to those that were previously infected.
The conclusion?
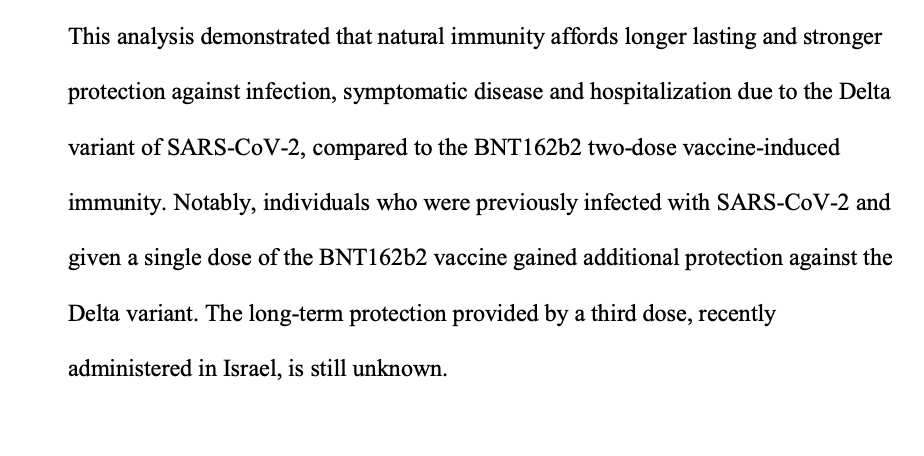
This study demonstrated that natural immunity confers longer lasting and stronger protection against infection, symptomatic disease and hospitalization caused by the Delta variant of SARS-CoV-2, compared to the BNT162b2 two-dose vaccine-induced immunity.
Data and Selection Criteria
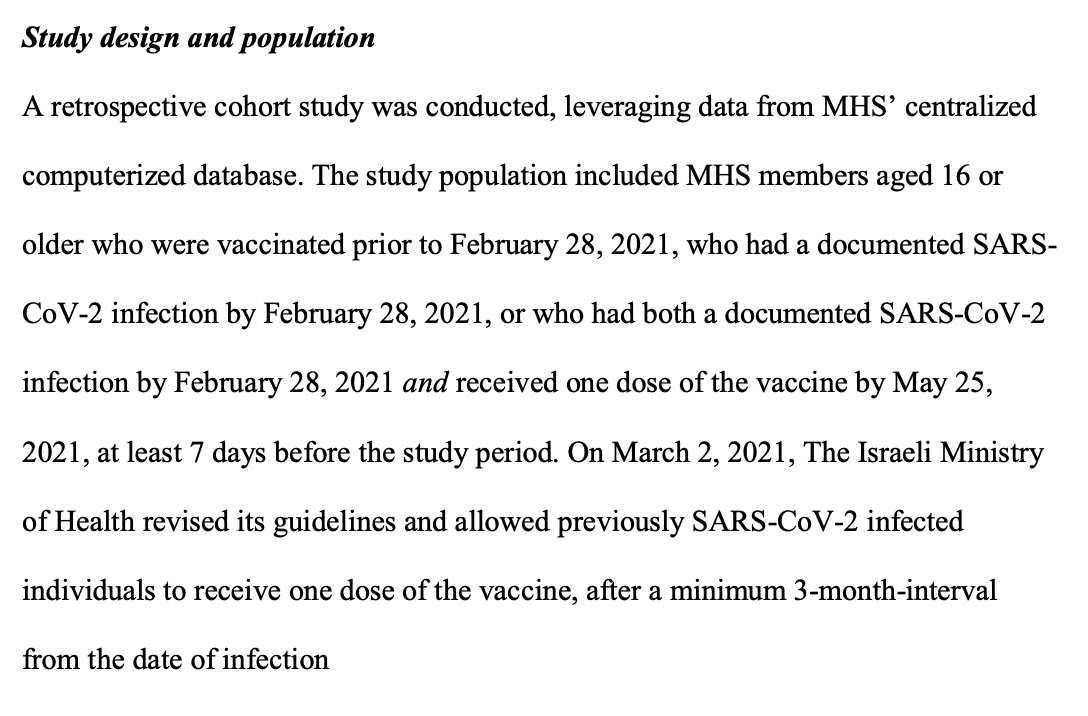
The data for this study come from the Maccabi Healthcare Services (MHS) which is Israel's second largest Health Maintenance Organization that has 2.5mm members (26% of the Israeli population) and provides a representative sample of the total Israeli population since membership in one of the four health funds is mandatory and the funds are prohibited from denying membership to any member. From this anonymized, longitudinal database the researchers then applied a selection criteria in order to limit the study population.
As Francois Balloux pointed out on Twitter there are likely to be some subtle biases in the data given the way the selection criteria were applied. That said, the samples are very large (n=16,215 for Model 1, n=46,035 for Model 2, and n=14,029 for Model 3) and so the results are more than likely genuine. That said, I would have liked to have seen a power analysis (I suspect it is properly powered, but better to verify!).
Methodology
Using this data, the researchers then conducted a retrospective cohort study which is basically where you are analyzing whether there was a risk of disease that was significantly different between exposed and non-exposed patients.
In this case the study population was split into 3 groups:
- 1) fully vaccinated and SARS-CoV-2-naïve individuals, namely MHS members who received two doses of the BioNTech/Pfizer mRNA BNT162b2 vaccine by February 28, 2021, did not receive the third dose by the end of the study period and did not have a positive PCR test result by June 1, 2021
- 2) unvaccinated previously infected individuals, namely MHS members who had a positive SARS-CoV-2 PCR test recorded by February 28, 2021 and who had not been vaccinated by the end of the study period
- 3) previously infected and vaccinated individuals, including individuals who had a positive SARSCoV-2 PCR test by February 28, 2021 and received one dose of the vaccine by May 25, 2021, at least 7 days before the study period.
The key dependent variables in the analysis were PCR confirmed COVID infection, COVID infection, COVID-related hospitalization, and COVID-related death. From here the researchers specified logistic regressions where they use the study groups as independent variables and the 4 SARS-CoV-2 outcomes as dependent variables.
Results
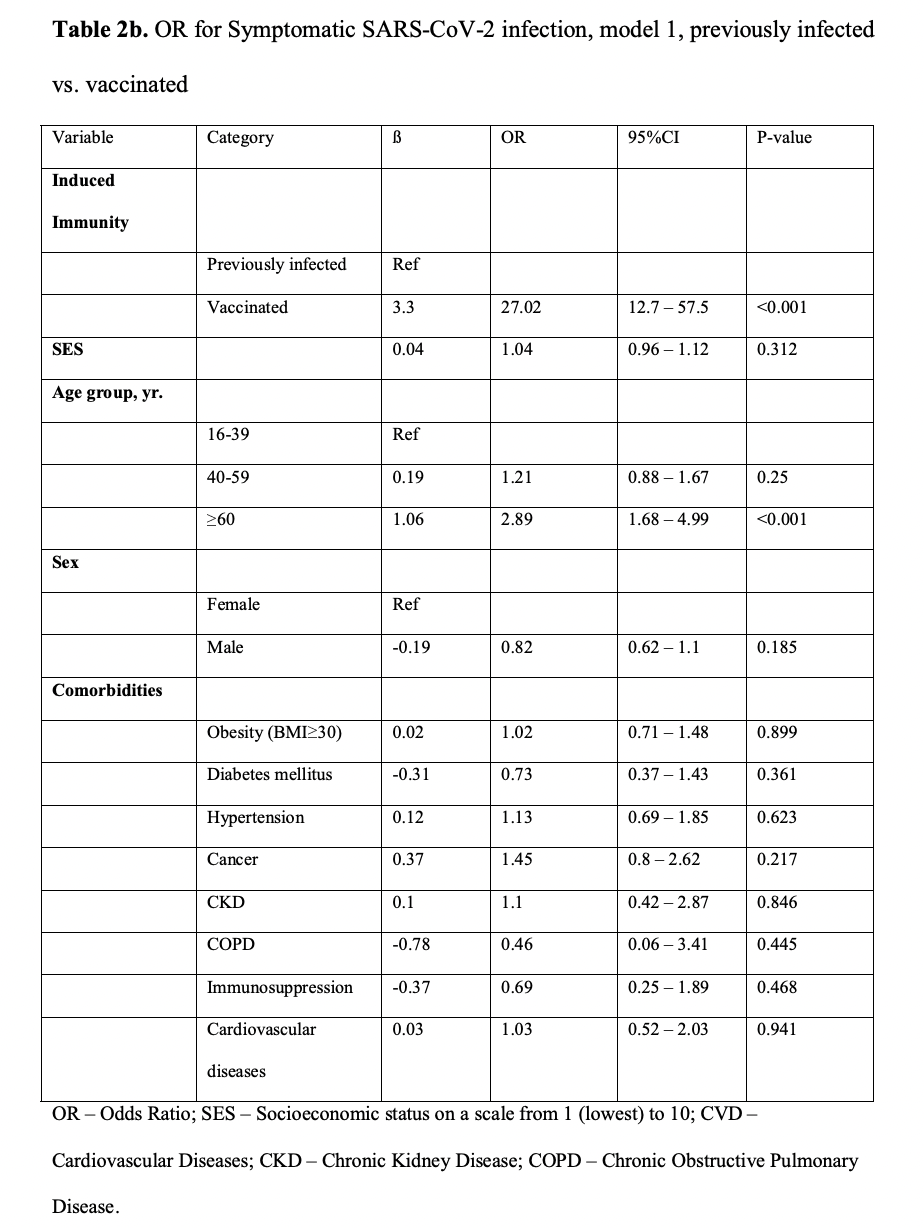
Model 1 – previously infected vs. vaccinated individuals, with matching for time of first event
- After adjusting for comorbidities, we found a statistically significant 13.06-fold (95% CI, 8.08 to 21.11) increased risk for breakthrough infection as opposed to reinfection (P<0.001).
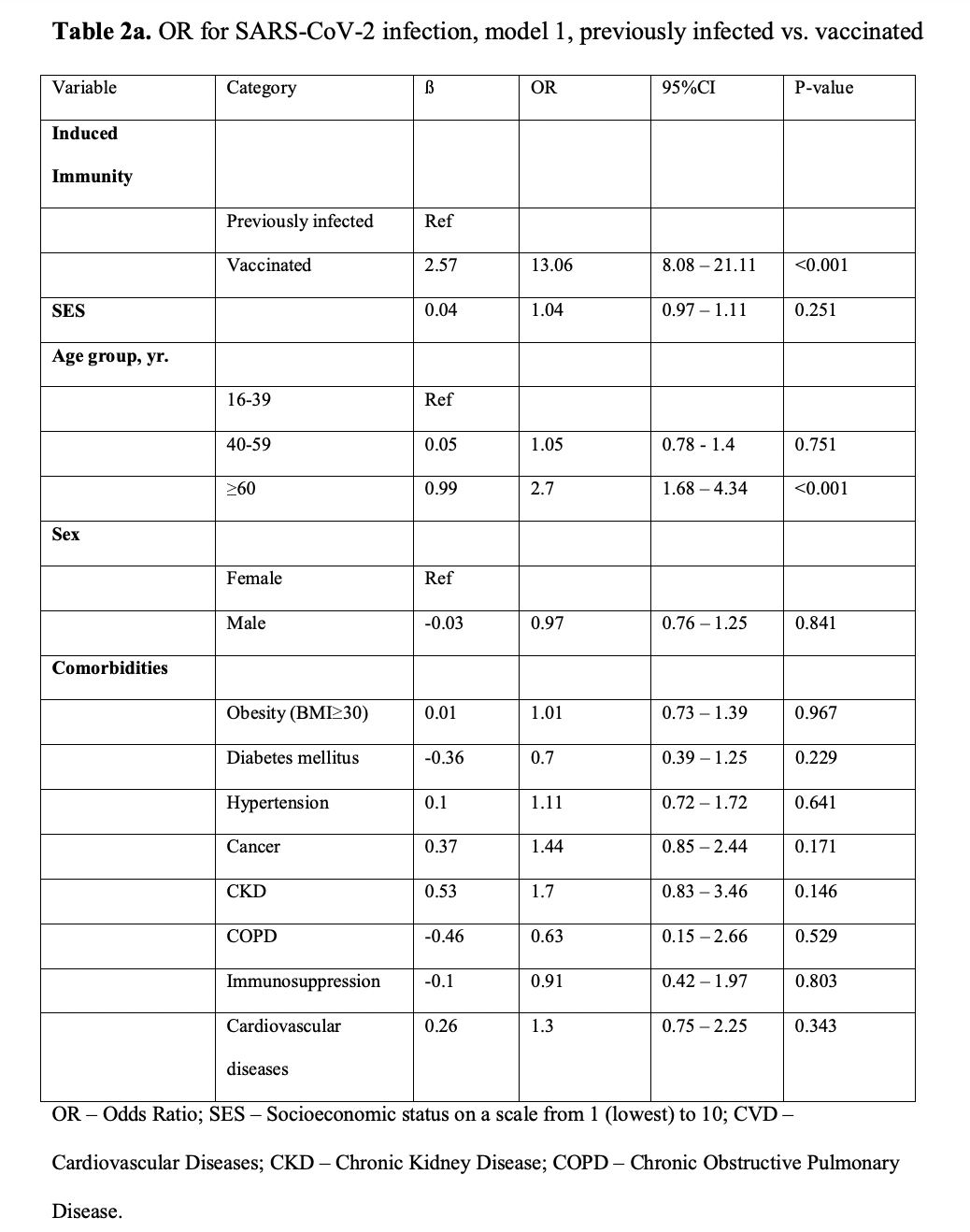
- After adjusting for comorbidities, we found a 27.02-fold risk (95% CI, 12.7 to 57.5) for symptomatic breakthrough infection as opposed to symptomatic reinfecting (P<0.001)
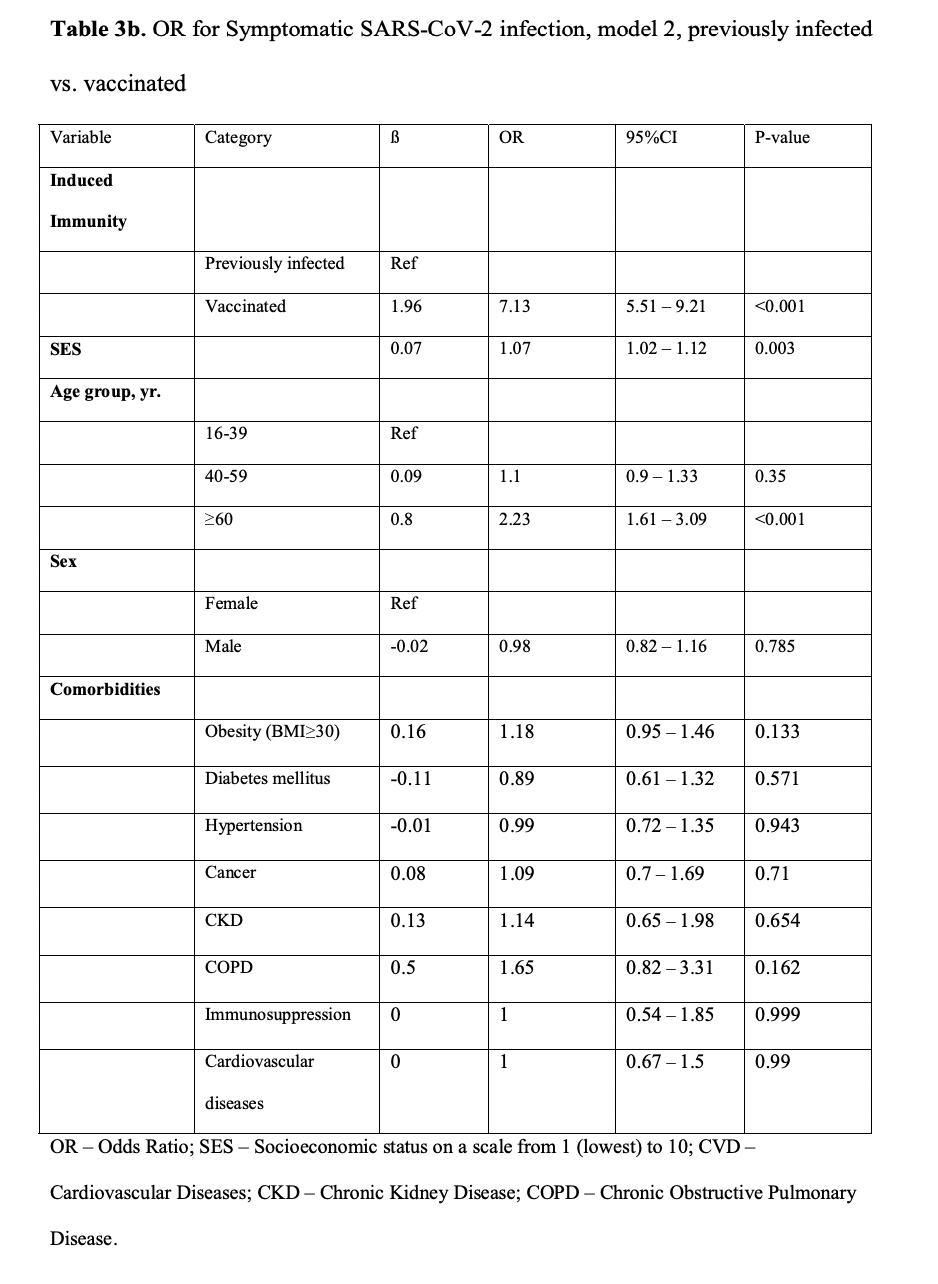
Model 2 –previously infected vs. vaccinated individuals, without matching for time of first event
- After adjusting for comorbidities, a 5.96-fold increased risk (95% CI, 4.85 to 7.33) increased risk for breakthrough infection as opposed to reinfection could be observed (P<0.001)
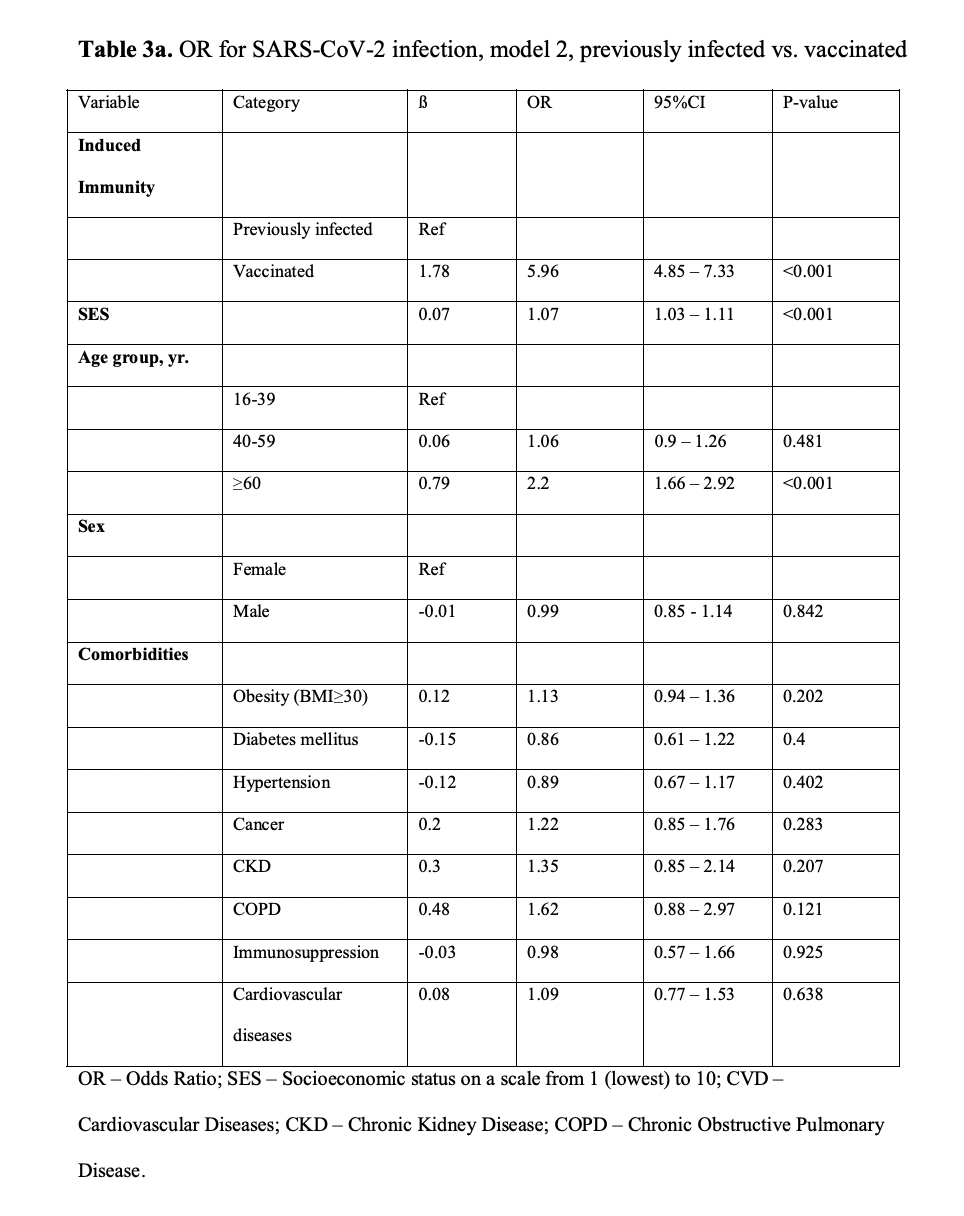
- Overall, 552 symptomatic cases of SARS-CoV-2 were recorded, 484 in the vaccinated group and 68 in the previously infected group. There was a 7.13-fold (95% CI, 5.51 to 9.21) increased risk for symptomatic breakthrough infection than symptomatic reinfection
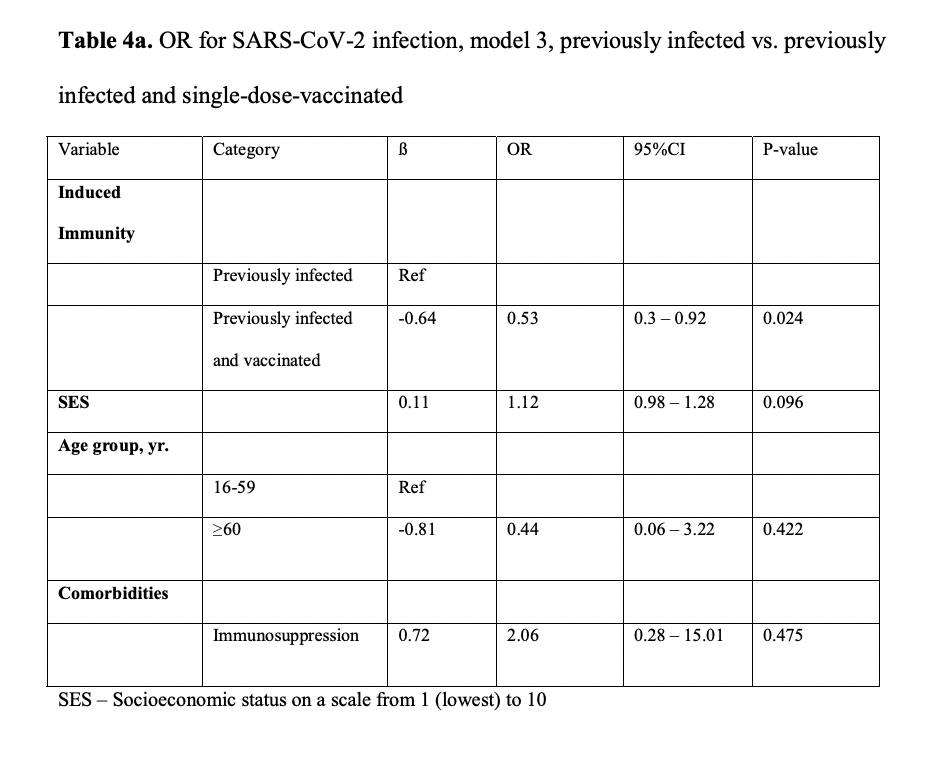
Model 3 - previously infected vs. vaccinated and previously infected individuals
- Examining previously infected individuals to those who were both previously infected and received a single dose of the vaccine, we found that the latter group had a significant 0.53-fold (95% CI, 0.3 to 0.92)
Takeaways
In the next week or so, I'm sure researchers will be going through the data to try and reproduce the figures cited here (that's why it's a pre-print). Assuming all that checks out, there are a couple interesting takeaways from this data:
- People who were never infected with SARS-CoV-2 and were vaccinated with 2 doses have a 13x increase in their risk of breakthrough infection with Delta.
- Compared with the previously infected, the SARS-CoV-2-naïve vaccinees had a 5.96x risk of breakthrough infection, a 7.13x risk for symptomatic disease, and a greater risk of hospitalization.
In short, if you got COVID and survived, the antibody response that your body mustered affords stronger protection against Delta than one induced through a 2-dose regimen of the Pfizer vaccine.